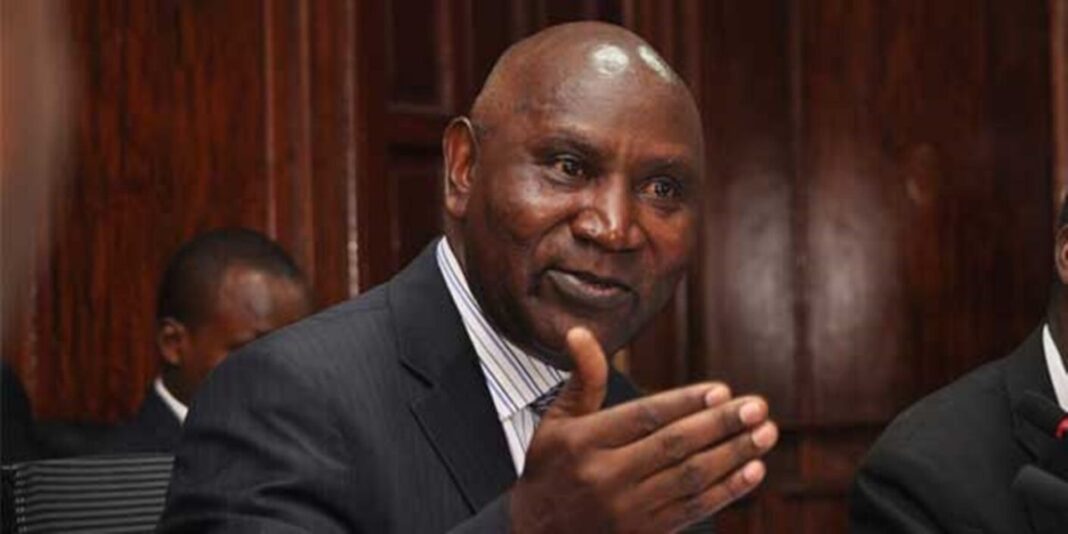
The government has admitted that Kenyans cannot access 36 specialised medical services within the country. In a Gazette Notice dated September 19, Health Cabinet Secretary Aden Duale said these services will only be available overseas under the new Social Health Insurance scheme.
The move exposes gaps in Kenya’s health sector, especially in advanced surgeries and therapies. While the government has promised to support patients, it has also capped the overseas medical cover at Ksh500,000 per person.

Health Services Unavailable in Kenya and What It Means for Patients
The Ministry of Health revealed that Kenya lacks facilities and training for complex joint replacements, paediatric procedures, and advanced therapies. These gaps force patients to travel abroad for treatment.
Duale announced that only patients who have updated their Social Health Insurance contributions will qualify for the overseas cover. The cover, however, has strict limits. A patient will not receive more than Ksh500,000, regardless of the procedure. The Claims Management Office will review every referral to ensure compliance with both medical and financial guidelines.
According to Duale, the decision aims to give Kenyans access to critical procedures while ensuring “value for money and quality care.” The announcement followed recommendations from the Benefits Package and Tariffs Advisory Panel, which listed the unavailable services.
Joint and Limb Replacement Procedures Missing in Kenya
The largest portion of the unavailable services involves advanced joint and limb replacement surgeries. Kenya lacks specialised joint replacement centres and enough training to perform these operations.
Among the missing procedures are:
- Wrist and metacarpal arthroplasty
- Ankle joint arthroplasty
- Proximal and distal femoral replacements
- Proximal tibial replacement
These gaps mean Kenyans with severe joint damage must look outside the country for relief. Without overseas support, many patients would suffer permanent disability.
Paediatric Procedures and Specialised Therapies Absent
Children needing advanced medical interventions face an even bigger challenge. Kenya currently does not provide paediatric liver or kidney transplants, bone marrow transplants, or laryngeal transplants.
Other missing procedures include:
- Intrauterine blood transfusion
- Shunt placement for bladder obstruction
- Vesicocentesis, thoracentesis, and paracentesis
- Fetoscopy and amniotic band ligation
- Laser ablation and amnioreduction
- Amnioinfusion, foetal reduction, cord occlusion, and cordocentesis
For therapies, Kenya does not offer several advanced cancer and regenerative treatments. These include:
- Peptide Receptor Radionuclide Therapy with Lutetium-177
- DOTA-TATE scans
- Fibroblast Activation Protein Inhibitor PET/CT imaging
- Microwave ablation of metastatic tumours
- Yttrium-90 radioembolization
- Chimeric Antigen Receptor T-cell therapy
In addition, services like sacral neuromodulation for urinary and faecal incontinence, surgical repair of birth-related brachial plexus injuries, photopheresis, nerve ablation therapy, neural regenerative therapy, and proton therapy are unavailable.
A Costly Reality for Kenyan Families
The government has tried to present the cap of Ksh500,000 as a fair balance between cost and care. But medical experts say that many of the listed procedures can cost millions of shillings abroad. Families may still be forced to raise extra money to cover the balance.
The Ministry of Health insists the new Social Health Insurance framework will reduce inequality by giving every Kenyan a chance to access specialised care. Yet, critics argue that the move highlights years of underinvestment in local health infrastructure.
Duale defended the government’s plan, saying the list was prepared after consultations with key stakeholders. He added that the long-term goal is to develop local capacity so that Kenyans will not have to travel abroad for treatment in the future.
For now, Kenyans who need any of the 36 listed procedures must rely on a system that offers partial support but not full relief. The reality is that without additional personal funding, many families will remain unable to access these life-saving treatments.